About
National Liver Utilisation Audit Proposal
On behalf of the NHSBT Clinical Leads in Organ Utilisation and the UK Liver Transplant Research Collaborative
Background
Organ utilisation is defined by NHSBT as ‘the action of making practical and effective use of organs from identified potential deceased donors’. It is well documented that the past two decades have witnessed a substantial increase in the number of deceased organ donors in the UK. Unfortunately, this has not been matched by a corresponding increase in the number of transplants (Figure 1).
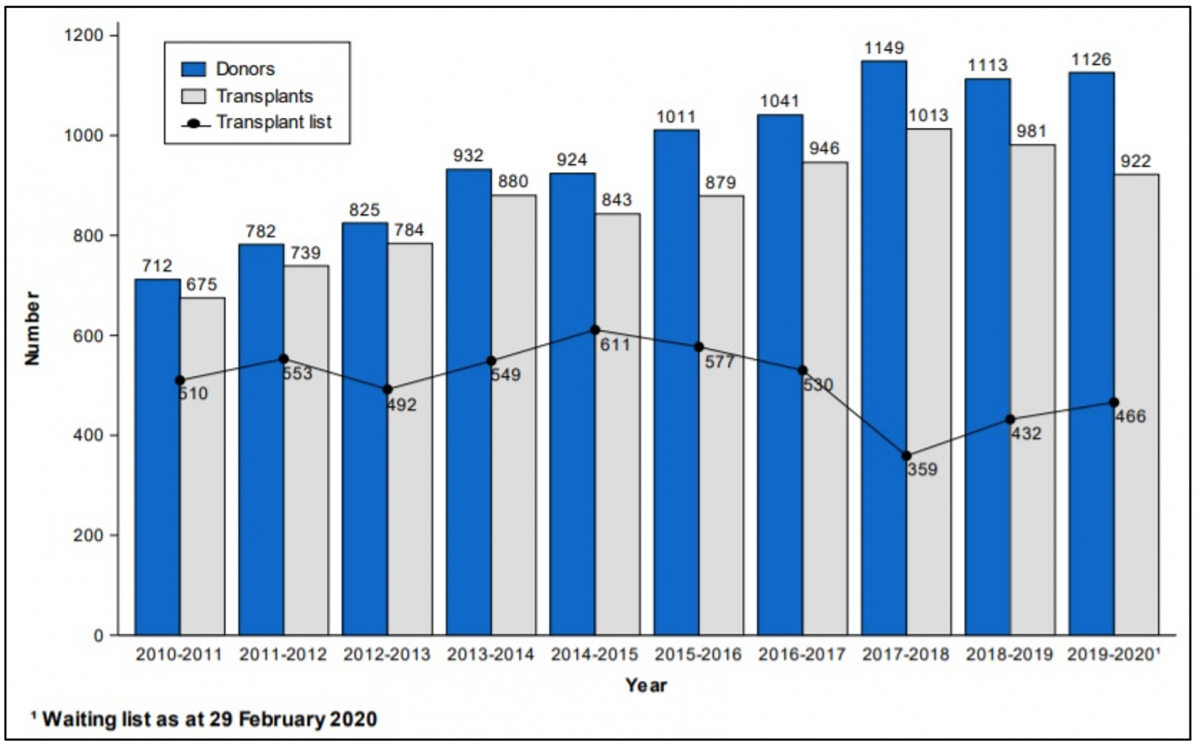
Figure 1: UK deceased donor liver transplant activity 2010-2020. Source: NHSBT Liver activity report Sept 2019
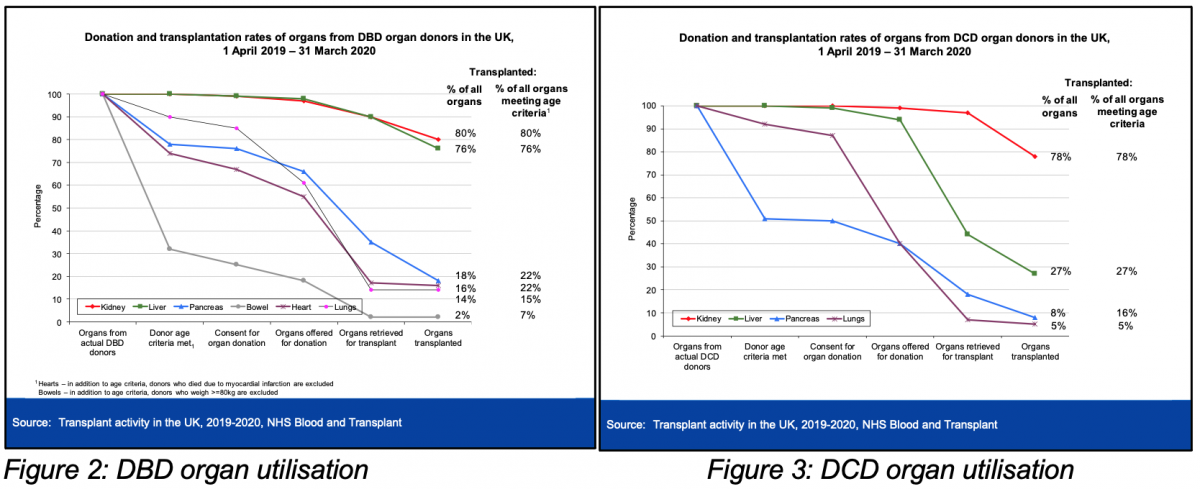
Of the donor organs which meet basic transplantability criteria only 76% of eligible DBD livers and 27% of DCD livers are ultimately transplanted (Figures 2 & 3). Part of this discrepancy can be accounted for by donor characteristics, with a greater proportion of the donor population being considered marginal either due to donor type (DCD) or other characteristics (age, co-morbidities, prolonged ITU stay etc.).
Concerns
There is a growing concern from the UK liver transplant community that other factors beyond those related specifically to the donor or recipient are impacting to a greater degree on the ability of individual units to be able to use an organ. These relate particularly to the logistical complexities of transplantation, with competing interests presenting obstacles to the donation-retrieval-preservation-transplantion process at every stage. At the donor hospital the pressure for ITU beds can potentially impact on the willingness for the local team to perform brainstem death testing, the urgency with which the organs must be offered or even whether or not a donor family are approached. The increasing national donor activity means that multiple retrieval teams are often active simultaneously across the country, potentially delaying when a retrieval can start. The retrieval team must compete with other emergency cases in the local theatre complex, with an organ retrieval given low priority and often delayed to accommodate other activity. There are disparities in access to novel organ preservation methods between different transplant teams, including access to NRP, NMP and HOPE techniques. At the recipient centre transplant activity may be limited by availability of clinical personnel, of ITU beds or lack of theatre space if multiple organs have been accepted.
Organ donation has become progressively more prolonged over the past decade (Table 1) with the time taken from donor referral to the start of organ retrieval increasing by over 50% from 2010 to 2016.
Table 1: Average time of UK organ donation process. Source: NHSBT Taking organ utilisation to 2020
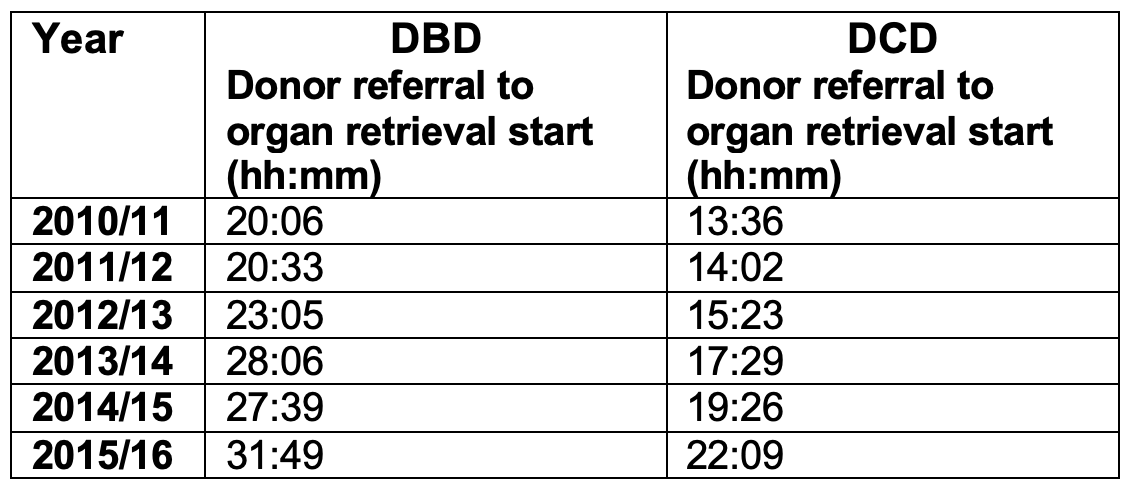
Organ retrieval has traditional been a nocturnal process, partly dictated by the length of time taken from donor referral to mobilization of retrieval teams, as well as by timing for access to emergency theatres. The progressive prolongation of this process has a knock-on effect on transplantation activity, pushing the retrieval activity towards daytime hours and the transplant procedure towards becoming an out-of-hours activity. Such a long, drawn-out process also makes it more challenging for transplant teams to plan their activity, with transplant theatres being put on hold whilst awaiting news of retrieval activity, potentially preventing other organs being accepted as well as compromising theatre activity in the transplant centre itself.
Existing data
Identifying which, if any, of the factors described above is hindering organ utilisation will be vital if structural changes are to be implemented to optimize the donation and transplantation process. NHSBT collects a large amount of data related to the organ donation and transplantation process. This includes detailed information about the reasons for non-utilisation of organs. In recent years these reasons for organ decline have been updated to be more comprehensive in the information that is recorded and also to better reflect the complexities of transplantation. This data is often entered many hours after the organ declining event and is rarely entered by the clinician who made the decision. As a result, the reliability of this data has often been called into question, although whether such cynicism is justified is unknown.
Audit design
This prospective study will include all seven UK liver transplant centres and will run continuously for a three month period from 1st February 2021 to the 30th April 2021. All donors from whom the liver is offered for consideration of transplantation in an adult recipient will be included. When livers are declined by multiple centres the reasons provided by each centre will be recorded. Whilst centre identification data will be recorded for each decision to decline a liver, individual clinician details will not be collected.
On a weekly basis, basic donor demographic data will be requested from NHSBT for the previous week’s liver donors to ensure that a record has been entered for every declined liver. On completion of the 3 month enrollment the decline reason data for all donor’s from the previous three months will be requested from NHSBT. These will be compared with the comprehensive data obtained from the present audit.
The Case Report Form of the audit is available here.
Data entry
Audit data will be entered within 48 hours of organ offer on to our secure and encrypted data entry management system.
It will be the responsibility of the Clinical Lead for Utilisation (CLU) at each site to ensure timely, accurate and comprehensive data collection. It is assumed that each CLU will identify colleagues at their transplant centre to whom aspects of the data collection will be delegated.
